[Surgery] Breast ductoscopy
Release time: 21 Jan 2025 Author:Shrek
Maybe you have heard of gastroscopy, colonoscopy, and laparoscopy. Have you heard of breast endoscopy? Today we will talk about the ductoscope, which has the smallest diameter among current endoscopes!
The magic tool to find out the cause of nipple discharge
Nipple discharge is one of the common symptoms in breast clinics, and it is easier for patients to notice. It is one of the main reasons why about 10% of clinical patients come to see a doctor. Nipple discharge is mainly caused by physiological factors, systemic diseases, breast diseases, etc. 5% to 10% of breast cancer patients have nipple discharge. Clinically, about 1% of breast cancers have nipple discharge as the first or only symptom. Since malignant lesions are more likely to cause bloody discharge, clinical patients with bloody discharge should be more alert to the possibility of malignant lesions. If male patients have nipple discharge, they should not take it lightly.
What is a ductoscopy?
The full name of breast ductoscopy is ultra-fine optical fiber breast duct endoscope. Its lens diameter is only 0.7mm, and its working injection channel is 0.3mm. The tortuosity is 40°, which can be used for branching at any level, including intraoperative operations, and at the same time injecting liquid medicine. treat. Designed based on Asian breast characteristics. The whole mirror body is made of cast water, which is safe and durable. Viewing angle: ≥70%, (excluding upper line) viewing angle 0°, can penetrate into six levels of milk ducts, without error, and can be used more than 200 times. Pixels: 6000 pixels, containing reinforced steel wire, not easy to break. The observation range is from the nipple duct opening to the distal end 5 to 6 cm, and the maximum insertion depth is (4.5 ± 1) cm on average, which can basically meet clinical needs. It can adapt to various disinfection measures and is very durable, reliable and safe. Working distance 6cm. Working hole: 0.3mm (SUS tube) can be equipped with biopsy, cell rotation biopsy equipment, pre-operative hooked positioning needle, and dredging guide wire.
Through the ductoscope, the doctor can see the lesions in the ducts at a glance. It is a cost-effective clinical diagnostic technology and has become the first choice method for diagnosing the cause of nipple discharge. Since 2009, breast ductoscopy has been used clinically to replace breast ductography.
Why do you need a breast ductoscopy?
1. Some nipple discharge is only caused by chronic inflammation in the milk ducts. After a clear diagnosis, only follow-up or regular drug irrigation under ductoscopy can avoid unnecessary surgery.
2. For space-occupying lesions in the ducts, ductoscopy can repeatedly observe them and accurately locate them. Provide surgical basis, ensure the accuracy of surgical location, and reduce the scope of surgery.
3. For early-stage breast cancer whose lesions are still limited to the ducts, ductoscopy is the earliest examination method that can detect its existence. Once discovered, early diagnosis and early treatment can be achieved.
Who needs a breast ductoscopy?
Common breast diseases, such as intraductal papilloma, ductal ectasia, ductitis, mammary gland hyperplasia and even breast cancer, can manifest as nipple discharge.
Generally speaking, patients with bloody or yellow discharge are more likely to have neoplastic lesions in the milk ducts. Patients with light yellow clear or turbid discharge are more likely to have chronic inflammation in the milk ducts. Patients with clear watery discharge are more likely to have mild inflammation in the milk ducts such as ductal ectasia.
If nipple discharge occurs, you need to see a hospital promptly. After consultation and physical examination by a breast specialist, a decision will be made whether a ductoscopy is needed based on the specific situation.
How to check breast ductoscopy?
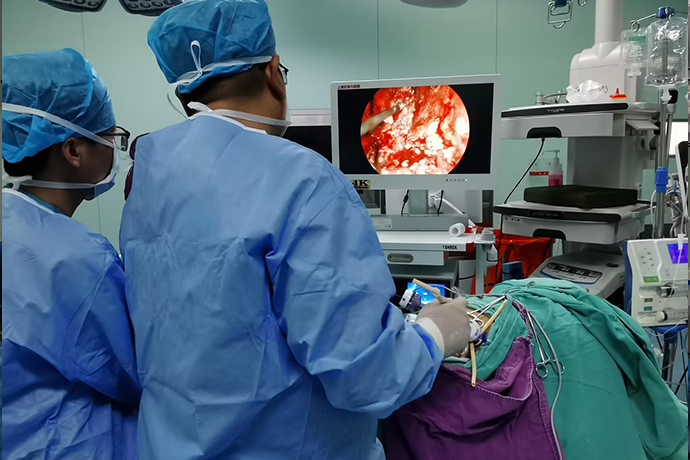
1. The patient lies flat throughout the procedure in a comfortable position. The patient is awake throughout the entire process and can see the examination process on the display screen with the doctor. The examination process takes about 3-5 minutes. After the examination is completed, the patient can leave and the report can be obtained on the spot.
2. At the beginning of the examination, after disinfection, the doctor will use a probe to expand the overflowing milk duct, then change the ductoscope to enter, inject anesthetics, physiological saline and other drugs through the working channel for flushing. Through the doctor's skillful operation, the entire milk duct can be clearly seen. Disease conditions within the milk ducts.
3. If new organisms, tube wall stenosis, bleeding, or suspected lesions are found in the catheter, the doctor will adjust the angle of the mirror and the brightness of the light source, observe carefully repeatedly, record the specific location, and take pictures on the spot to provide information for the next surgical treatment. Diagnosis basis and precise positioning.
Is breast ductoscopy painful?
Breast ducts are indeed very thin, but the ductoscope lens is also very thin. Moreover, patients with discharge usually have varying degrees of dilation of their milk ducts, so there is no pain or only mild pain.
What should I pay attention to before and after breast ductoscopy?
1. First of all, relax your mentality during the examination. Breast ductoscopy is a non-invasive examination. It enters the physiological channels that already exist and will not cause damage to the human body.
2. The nipple is obviously red and swollen locally. Breast ductoscopy should be avoided during the acute inflammation stage.
3. Try to avoid breast ductoscopy during menstruation.
4. Patients with serious medical diseases need to wait until their condition stabilizes before undergoing breast ductoscopy.
5. Patients with fever caused by any reason on the day of examination cannot undergo breast ductoscopy.
6. Bathing is prohibited for 24 hours after the examination.
Breast ductoscopy can directly observe the changes in the milk duct epithelium, and can make qualitative and localized diagnosis of small lesions in the milk ducts with bloody or serous discharge from the nipple but no tumor in the breast. It is an important clinical examination method for breast diseases.
Scope of application for breast ductoscopy
1. Various nipple discharges
Especially for patients with unilateral or single-hole nipple discharge, bloody nipple discharge, and yellow discharge, the incidence of neoplastic lesions in the milk ducts is about 1/3 to 1/2. In addition, patients with white or colorless discharge also have There are many cases caused by tumors in the breast ducts, which require surgical treatment after ductoscopy.
2. Areola area tumors accompanied by nipple discharge
Most of the tumors in this area are caused by tumors in the milk ducts and are closely related to the milk ducts. Breast ductoscopy can identify the diseased milk ducts, thereby guiding the operation, accurately removing the tumors and diseased milk ducts, and reducing the chance of local recurrence after surgery. .
80% of breast cancer patients are first diagnosed with breast lumps. Patients often discover breast lumps inadvertently, which are mostly single, hard, with irregular edges and smooth surfaces. Most breast cancers are painless lumps, and only a few are accompanied by varying degrees of dull pain or stinging pain.
3. Patients with periareolar plasma cell mastitis
Plasma cell mastitis is caused by the blockage of the proximal end of the milk duct and the accumulation of secretions, exfoliated cells, and inflammatory cells in the milk duct, resulting in acute or chronic inflammation of the breast. Breast ductoscopy can lavage and collect exfoliated cells in the milk ducts for cytological examination to confirm the diagnosis. At the same time, it can also flush and clear the diseased milk ducts to achieve the purpose of drainage. In addition, if the inflammation is relatively localized, the diseased milk ducts can also be identified under a ductoscope and the diseased milk ducts can be surgically removed.
4. Mastodynia
Mastodynia is a type of breast hyperplasia, which is partly caused by blockage of the proximal milk ducts, resulting in poor drainage and distortion of the distal milk ducts. Performing duct lavage under ductoscopy to clear the milk ducts can help A clear diagnosis can be made and a certain therapeutic effect can be achieved.
5. Skin changes
Skin changes caused by breast cancer can cause a variety of signs. The most common is that the tumor invades Cooper's ligament, which connects the breast skin and the deep pectoral muscle fascia, causing it to shorten and lose elasticity, pulling the skin of the corresponding part, and a "dimple sign" appears. That is, a small depression appears in the breast skin, like a dimple. If cancer cells block lymphatic vessels, "orange peel-like changes" will occur, that is, many small dot-like depressions will appear on the breast skin, just like orange peel. In the late stage of breast cancer, cancer cells infiltrate into the skin along lymphatic vessels, glandular ducts or fibrous tissue and grow, forming scattered hard nodules in the skin around the main cancer focus, which are so-called "skin satellite nodules".
6. Swollen axillary lymph nodes
More than 1/3 of breast cancer patients admitted to large hospitals have axillary lymph node metastasis. In the early stage, swollen lymph nodes in the ipsilateral axilla may appear. The swollen lymph nodes are hard, scattered, and pushable. As the disease progresses, the lymph nodes gradually fuse and become adherent and fixed to the skin and surrounding tissues. In the late stage, metastatic lymph nodes can be felt on the supraclavicular and contralateral axilla.
Breast ductoscopy is an examination and treatment that uses human physiological channels. It is truly non-invasive and scarless. You are awake throughout the treatment process and can observe the images and understand the condition under the doctor's explanation. Generally, there is no need to change the dressing after the treatment.

- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- 【4K Basics】4K Ultra HD Endoscope Camera System
- 【General Surgery Laparoscopy】"Two-step stratified method" operation flow of left lateral hepatic lobectomy
- 【General Surgery Laparoscopy】Left Hepatectomy