[Gynecological laparoscopy] Causes and treatment of urinary system injuries
Release time: 19 Feb 2025 Author:Shrek
The anatomical relationship between the female reproductive system and the urinary system is closely adjacent. During gynecological surgery, due to the invasion of malignant tumors, severe adhesions of pelvic organs, or large tumors in the pelvic and abdominal cavity, the anatomical position of the urinary system can be changed and the tissue layer is unclear, which can easily cause damage to the urinary system. Although there is currently no systematic review comparing the incidence of urinary tract injuries between open and laparoscopic surgery.
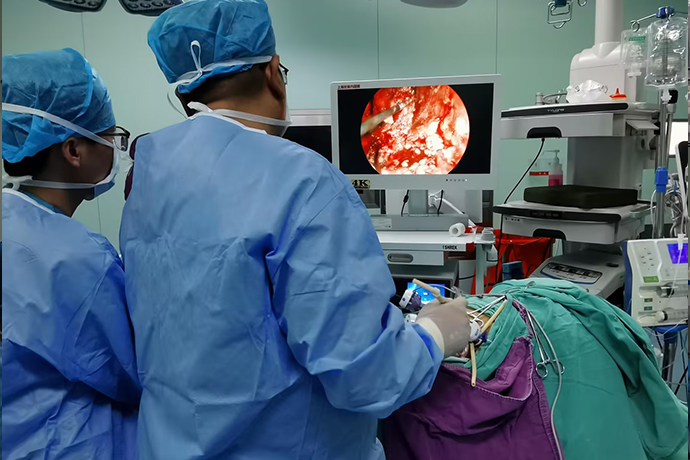
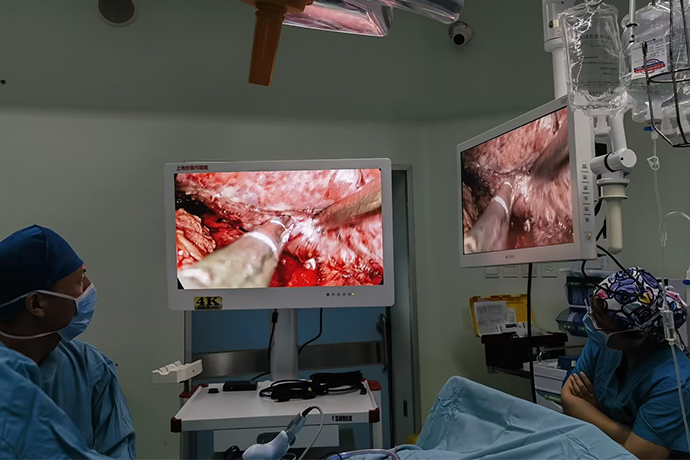
In clinical practice, more and more benign and malignant gynecological surgeries can be completed under laparoscopy. However, with the expansion of gynecological laparoscopic surgery applications and the increase in surgical difficulty, the incidence of intraoperative and postoperative complications has also shown an upward trend. Severe irreversible damage will have a serious impact on patients' postoperative quality of life.
Causes of Urinary System Damage
Urinary tract injury is one of the most common complications of laparoscopic surgery.
Since laparoscopic surgery often uses electrocoagulation and electrocution to treat blood vessels and tissues, the local temperature can reach as high as 300°C. Especially when a single-stage electric hook is used to perform electrocoagulation and resection near the ureter, the heat conduction effect can spread to the surrounding area as far as 2cm, causing ischemic necrosis of the ureter. This kind of thermal injury is often not easy to detect during the operation, but the corresponding symptoms and signs appear some time after the operation. Once an abnormal increase in drainage volume is found, the possibility of urinary system fistula should be considered. It is usually considered in two steps. First, it is necessary to determine whether there is a urinary system fistula, and secondly, it is necessary to determine the location of the fistula.After surgery, the creatinine and urea nitrogen indicators of the pelvic drainage fluid can be checked to determine whether there is a urinary system fistula; the bladder methylene blue test can be used to determine whether it is a vesicovaginal fistula or a ureterovaginal fistula; further cystoscopy and CT urinary tract imaging (CTU) can be performed to determine the side of the injury and the location of the fistula. It is necessary to pay attention to whether there are compound fistulas, that is, there are ureteral fistulas and bladder fistulas at the same time, bilateral ureteral fistulas, and more than two bladder fistulas.
Intraoperative and postoperative management of ureteral injury
When the tubular cord is found to be cut or injured during the operation, or there is a lot of exudate in the surgical field, the source of the exudation should be carefully searched to identify the ureteral injury. If it is confirmed that the ureter has been accidentally tied or clamped, it should be removed immediately. If the clamping or suturing time is short and the damage is not obvious, the ureter can be left for a period of time to observe the ureteral peristalsis. The ureteral peristalsis is good and does not need to be treated. If the injury is obvious and the peristalsis function is lost, it should be treated as appropriate. In mild cases, double "∵J" ureteral catheters can be placed. In severe cases, end-to-end ureteral anastomosis or ureterovesical anastomosis can be considered after cutting off.
If the ureter is found to be severed or seriously injured during the operation, end-to-end ureteral anastomosis can be performed if the position is higher. Drainage is placed next to the anastomosis. At the same time, a double "J" ureteral catheter is placed in the ureter, and the upper end to the lower end of the renal pelvis is placed in the bladder. The catheter is removed through a cystoscope 2 weeks after the operation. If the location of the injury is low, ureterovesical anastomosis can be performed, and a double "J" ureteral catheter can also be placed, and the catheter can be removed through a cystoscope 2 weeks later.
Different treatment methods are selected based on the patient's general condition, the location of the injury, the scope of the defect, local blood supply, infection or not, etc. If there is no obvious obstruction to the IVU, and the retrograde intubation is unobstructed, there is no chills, fever, and little urine leakage, double "J" tube drainage and anti-infective conservative treatment can be given for 10-14 days. Once ureteral dilatation occurs, ureterovesical reimplantation or other treatments should be performed promptly to save renal function. For those with serious injuries, the injured part should be resected decisively, and the ureters should be anastomosed end-to-end or transplanted into the bladder and double ""J tubes should be placed for 4-6 weeks. For early ureteral fistulas with small postoperative urinary fistulas, ureteral catheters can be placed for continuous drainage for 10-14 days, and healing is possible. When it is difficult to place a large fistula or double "J" and conservative treatment is ineffective, a ureteral stent or nephrostomy is performed, and a second-stage repair is performed 3 to 6 months after the operation.
Characteristics, prevention and treatment of bladder injuries
1. Features
The incidence rate of bladder injury is about 0.34%, and the injury locations are mainly the top, bottom and trigone of the bladder. Causes of injury include: 1) poor technique and unclear anatomical levels; 2) thermal damage to instruments [6; 3) various factors that lead to local adhesion, such as cervical tumor infiltration, history of cesarean section, endometriosis, reproductive system tuberculosis, inflammatory reactions, etc., which not only increase the difficulty of the operation, but also increase the probability of bladder damage during the separation of the bladder-cervicovaginal space1. Hong et al retrospectively analyzed 118 cervical cancer patients who underwent laparoscopic radical hysterectomy. Bladder injury occurred in 10 cases (8.47%), of which 5 had a history of cesarean section, resulting in damage to the bladder base and trigone area.
2. Prevention
2.1 Anatomy
The bladder is composed of mucosal layer, muscular layer and adventitia, and the outer membrane surface is covered by peritoneum. The peritoneum is tightly connected to the adventitia at the midline of the bladder tip and upper body, but is loosely connected to the adventitia on the side of the bladder body, making the peritoneum easy to peel off. This is the anatomical basis for extraperitoneal dissection to reach the lower uterine segment. There is a thin layer of loose connective tissue gap between the bladder and cervix, located between the bladder trigone and the cervix. Its upper boundary is the vesicouterine reflexed peritoneum, its lower boundary is the superior vaginal septum, and both sides are the medial leaves of the vesicocervicovaginal ligament. The vesicovaginal gap can be regarded as a downward continuation of the bladder and cervix gap. There are few blood vessels in it and it is easy to separate.
2.2 Precautions
In patients with no obvious adhesions in the lower uterine segment, open the bladder and uterus and fold the peritoneum, lift the uterine cup with force to expose the bladder-cervix-vaginal gap, gradually push the bladder down along the gap, separate and expand downward and on both sides, and reach a level sufficient for surgery. If the adhesion layer is unclear and the anatomical layer of the connective tissue gap between the bladder and cervix has not been clarified, an ultrasonic scalpel can be used to sharply separate the cervix as close as possible, combined with a blunt suction device to gently push down to feel the push-down tension, resistance and bleeding. If the tension and resistance are high and bleeding is easy, it often means that the anatomy is not good. At this time, you should not push hard to avoid separation and bleeding. You should separate sharply and find the correct limit, and then perform blunt separation v to avoid forced blunt separation, which may cause damage to the blood vessels of the bladder muscle layer, bleeding or even bladder rupture.If the tension or resistance is small and there is very little bleeding, it often means that the anatomical level is correct, and the white and smooth bladder-cervical fascia can be seen. At this time, the blunt downward push of the suction device will be more effective until it stops when the resistance increases, and then sharp separation is performed. Repeatedly, the bladder can be pushed down with less bleeding. For some patients with adhesions between the bladder and the lower uterus, you may consider opening the lateral fossa of the bladder first, bluntly and sharply separating the adhesions from the side of the bladder via an extraperitoneal approach, and then pushing down the bladder. However, attention should be paid to the anatomy of the lateral fossa of the bladder and not to damage the lateral wall of the bladder. Although there is no exact mechanism for fistula formation, experimental studies in animals by Cogan et al. have shown that the formation of vesicovaginal fistula after laparoscopic hysterectomy is related to unipolar thermal damage. Therefore, it is best to use an ultrasonic scalpel instead of unipolar when resecting the vaginal wall to reduce the possibility of thermal injury.
3. Processing
After the bladder is separated and moved, a timely examination should be carried out. If bladder damage is found, it should be repaired immediately. If there is a high degree of suspicion but no obvious damage can be seen, intraoperative injection of methylene blue solution or cystoscopy can be used to help diagnose R1. Only muscle layer injuries can be sutured with 4-O absorbable synthetic threads intermittently. If the break has been penetrated, two layers of suturing should be performed. After full-thickness suturing with 4-0 absorbable thread, one layer of inversion suturing is performed. When the break is located near the trigone area of the bladder, be careful not to injure the ureteral opening when suturing. Adequate bladder drainage for 2 weeks after surgery and prevention of infection can usually lead to primary healing.Most electrical bladder injuries are difficult to detect during surgery, usually manifesting as a large amount of vaginal discharge about one week after the operation or a small initial discharge that gradually increases and becomes infected. At this time, the presence of urinary fistula and its location should be determined through intravesical injection of methylene blue solution, retrograde cystourethrography, cystoscopy, B-ultrasound, and comparison of vaginal exudate and urine for creatinine, urea nitrogen, and electrolytes. As soon as it is discovered, an indwelling urinary catheter should be placed immediately for adequate bladder drainage to control urinary tract infection, and the patient should try to adopt a position that can reduce urinary fistula exudate. Most bladder injuries and vesicovaginal fistulas can be healed in the first stage without leaving sequelae. For vesicovaginal fistulas that are unsuccessfully conservative, secondary repair is usually performed 3 to 6 months after surgery.
- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- 【4K Basics】4K Ultra HD Endoscope Camera System
- 【General Surgery Laparoscopy】"Two-step stratified method" operation flow of left lateral hepatic lobectomy
- 【General Surgery Laparoscopy】Left Hepatectomy