[Laparoscopic Hepatobiliary Surgery] Splenomegaly
Release time: 30 May 2023 Author:Shrek
Compared with the liver, gastrointestinal tract and other internal organs in our abdomen, there is an organ that seems less important and easily overlooked. This organ is the spleen. There is a folk saying that "spleen weighs three or two", but you may not know it. Problems with a small spleen often indicate abnormalities in the body.

Some people find an enlarged spleen during physical examination. What are the harms of an enlarged spleen? Splenomegaly is divided into mild, moderate and severe. The etiology of splenomegaly is very complicated. Except for a few physiological splenomegaly, the cause should be found early under the guidance of a doctor. The causes of an enlarged spleen generally fall into the following categories:
1. Splenomegaly caused by various infectious diseases
For example, some special types of infections, such as typhoid fever, tuberculosis, bacterial endocarditis, schistosomiasis, etc. These diseases are relatively unfamiliar to urban residents, but in remote areas with poor sanitation conditions, spleen splenosis caused by infectious diseases Swelling is not uncommon.
2. Congestive splenomegaly caused by splenic venous reflux disorder
Liver cirrhosis will lead to portal hypertension secondary to portal hypertension, and a major feature of portal hypertension is splenomegaly, and it will also be combined with severe leukopenia, hemoglobin and thrombocytopenia, which seriously threatens the health of patients with liver disease; in addition, heart failure and other causes liver disease Congestion can also cause enlarged spleen.
3. Many blood system diseases are characterized by splenomegaly
For example, leukemia, lymphoma, hemolytic anemia, etc., the spleen may be very swollen.
4. Enlargement of the spleen itself and other diseases
Splenomegaly can occur in splenic cysts, hemangiomas, systemic lupus erythematosus, dermatomyositis, etc.
From the above, we can see that there are many reasons for splenomegaly. If it cannot be diagnosed and treated in time, the disease may be delayed. For patients with splenomegaly, it is necessary to go to a regular large hospital for a comprehensive examination. Then treat according to the diagnosis.
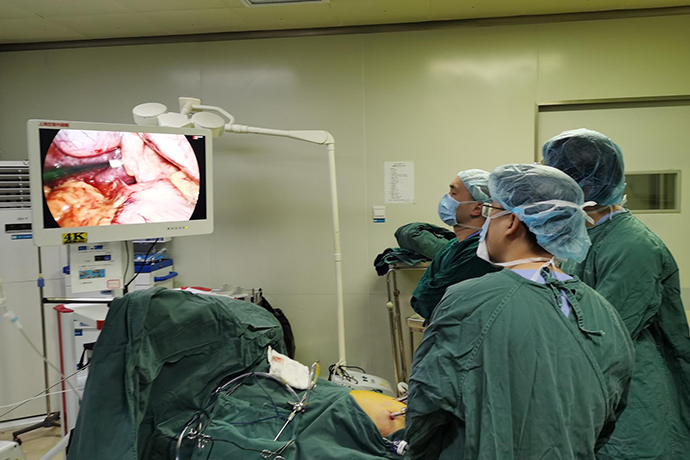
Splenectomy is a common clinical operation. Traditional splenectomy mainly uses laparotomy. The world's first laparoscopic splenectomy (LS) was successfully performed by Delaitre in 1991. Compared with traditional surgery It has the advantages of light patient pain, small surgical trauma, fast postoperative recovery, short hospital stay, and few postoperative complications. carry out. Safe and effective treatment of the splenic pedicle is the key to the success of LS. Currently, laparoscopic splenectomy by secondary pedicle division (LSSP) and primary splenic pedicle division are mainly used for the treatment of the splenic pedicle in laparoscopic splenectomy. , that is, laparoscopic splen-ectomy by Endo-GIA division (LSED) two surgical methods, both of which have their own advantages and disadvantages, how to choose the appropriate method has become a research hotspot at home and abroad.
Puncture hole position in laparoscopic spleen surgery
Each Trocar hole should be selected according to the size of the spleen, the lower pole of the spleen, and the position of the splenic hilum after the laparoscope is inserted (the position of the poking hole will be different from the original preset position after the abdominal cavity is inflated).
Basic principle: With the hilum of the spleen as the center, the piercing holes are distributed in a fan shape, and the position and direction of each hole should also take into account the incision needs when converting to laparotomy.
According to different body positions and the position of the lower border of the spleen, select the common position.
Intraoperative exploration
When performing splenectomy for chronic diseases, it is necessary to investigate the cause of the preoperative diagnosis, including the size of the spleen, whether there is adhesion, whether there is an accessory spleen, the relationship with the surrounding organs, and the condition of the splenic artery and vein. In cases of cirrhotic portal hypertension, attention should be paid to the size of the liver, the degree of cirrhosis, the presence or absence of new organisms, the amount of collateral circulation in the portal vein system, and the presence or absence of embolism, and the portal vein pressure should be measured. For cases of congenital hemolytic anemia, the gallbladder and bile duct should be detected to determine whether there are stones.
Selection of Surgical Instruments for Laparoscopic Splenectomy
In laparoscopic splenectomy combined with pericardial vascular dissection, more tissues and vessels need to be dissected, so equipment with better hemostatic effect should be selected. Among the many hemostatic devices currently available, Ligasure (Ligavessel Closure System) is more suitable for laparoscopic splenectomy combined with peripheral vascular detachment. It has less thermal damage and can completely and permanently close blood vessels with a diameter of less than 7mm. Ultrasonic scalpel is effective for coagulating blood vessels with a diameter of less than 3mm, but for portal blood vessels in portal hypertension, the effective coagulation diameter may be smaller. In this operation, it can be used to cut off the perisplenic ligament. When cutting off the short gastric blood vessels and the blood vessels around the spleen, the effect is poor and bleeding is prone to occur. Although the hemostatic function of electrocoagulation hook is worse than that of the above two, it is fast and accurate when freeing transverse ligaments without varicose vessels (such as splenocolic ligament).
"Gold Finger" is a rare and good instrument used to expose the surgical field during the operation, and it is a basic guarantee for the smooth and rapid operation. The part of the "golden finger" used for exposure is a rectangle. During the exposure process, it acts on a plane by "push, press, and support" to achieve a nearly perfect exposure effect, and it is not easy to damage organs and tissues and cause bleeding.
Autologous blood recovery technology can escort the operation. Intraoperative use can not only reinfuse and reuse the bleeding without loss, but also reinfuse and reuse the blood stored in the enlarged spleen. The spleen of such patients is an enlarged spleen, even a giant spleen, and there is usually a considerable amount of blood in the spleen. The advantages of autologous blood transfusion are:
(1) During the operation, the blood source can be obtained immediately and quickly, and the blood can be reinfused, and the hemoglobin value will not decrease due to bleeding
(2) Can effectively increase postoperative hemoglobin value
(3) Avoid or reduce intraoperative allogeneic blood transfusion and related complications
(4) It can alleviate the contradiction of blood tension to a certain extent
(5) It can relieve the psychological pressure of the operator during the operation, so that he can perform the operation more calmly
(6) Created better surgical conditions and opportunities for RH(-) patients
The approaches for splenectomy are generally divided into anterior approach (splenogastric ligament→splenocolic ligament→splenorenal ligament→splenophrenic ligament→splenic pedicle) and posterolateral approach (splenorenal ligament→splenocolic ligament→splenogastric ligament→splenic diaphragm). ligament → spleen pedicle).
1. Abdominal exploration revealed a huge cyst on the upper pole of the spleen.
2. Free the splenic artery and place a blocking band.
3. The upper pole branch of the splenic artery was freed, clamped and cut off.
4. Cut off the branch of the upper pole splenic vein.
5. The boundary line of blood supply occlusion can be seen clearly, and the pre-resection line can be determined.
6. Complete resection of the upper pole of the spleen and cysts, and strict hemostasis.
7. The residual spleen has a good blood supply.
Laparoscopic splenectomy (LS) is the gold standard procedure for removal of the spleen in elective patients. Laparoscopic surgery can also be safely used in patients with splenomegaly. Although many authors prefer a lateral approach, we place the patient in the supine position. This position provides good exposure of the splenic vessels and allows rapid control of hilar blood flow. Furthermore, the supine approach does not require retraction of the spleen from the hilum, allowing the procedure to be performed without the need for a fourth trocar in most cases. We control the hilar vessels, and after closing the main trunk of the splenic artery with a hem-o-lok, fire the endoscopic stapler with the vascular cassette in one shot, provided that the tail of the pancreas is protected and all hilar structures can be clamped with the stapler between mouths. We call this method the bookbinding technique. LS has the advantages of a short hospital stay, reduced postoperative pain, and low morbidity, but should be performed by skilled and experienced surgeons using standardized techniques.
Surgical Notes
Flushing, hemostasis
Take out the gauze pad of the spleen bed, carefully check the retroperitoneum, diaphragm surface, greater curvature of the stomach, and tail of pancreas, etc. If there is bleeding, it should be ligated to stop the bleeding. In patients with portal hypertension, there are many retroperitoneal collateral vessels, which are easy to ooze blood, and can be folded and sutured to stop bleeding. In the greater curvature of the stomach, when dealing with the short gastric vessels in the spleen and stomach, there may be damage to the gastric wall or bleeding. At this time, the seromuscular layer of the gastric fundus should be sutured along the greater curvature of the stomach to prevent bleeding or gastric leakage.
Order of operation
During the operation, follow the order of "from the periphery to the spleen hilum, from bottom to top, easy first and then difficult". When disconnecting the ligament around the spleen, damage to surrounding organs such as the stomach, colon, and diaphragm should be avoided. If the splenic-phrenic ligament is short and it is difficult to separate all the perisplenic ligaments, the splenic pedicle can be dealt with after separating the splenic colon and spleen-renal ligament, and then the remaining perisplenic ligaments can be separated.
Surgical field exposure
Do not pull the spleen violently during the operation, which may cause capsular hemorrhage and affect the operative field. Gently lifting the spleen with a suction or serpentine retractor is usually sufficient by an assistant.
Treatment of splenic pedicle
1. To deal with the spleen pedicle should be "steady, accurate and gentle". Ligate the arteries first and then the veins to avoid splenic congestion and enlargement caused by venous ligation first and increase the difficulty of the operation.
2. For the giant spleen, free the splenic artery at the upper edge of the pancreas before dealing with the splenic pedicle, and ligate or clip it. This allows the blood in the spleen to reinfuse itself, reducing the size of the spleen and reducing the risk of bleeding.
3. Avoid using titanium clips in the area where the linear cutter is to be lined, so as not to cause massive bleeding due to firing failure.
4. Vascular ligation can be treated with silk thread ligation, Hemolock, absorbable biological clips, and endoscopic linear cutting staplers such as EndoGIA or EC60. Or white nail bin.
Intra-abdominal hemorrhage
Usually occurs within 24-48 hours after surgery. The most common cause is severe hemorrhage from the diaphragm surface, detachment of the splenic pedicle ligation thread, or hemorrhage from vessels that were not ligated during the operation.
Preventive measures: during the operation, repeatedly check the diaphragm surface, the ligated end of the spleen-gastric ligament, the lateral abdominal wall, the retroperitoneum, the spleen pedicle, and the tail of the pancreas to see if there is any bleeding point, and strictly stop the bleeding.
Subphrenic abscess
Within 1 to 2 weeks after splenectomy, patients often have hypothermia, generally not exceeding 38.5°C. However, if the high fever persists after the operation, or if the body temperature drops and then rises after 1 week after the operation, it cannot be simply regarded as splenectomy fever. More than subdiaphragmatic hemorrhage or infection.
Preventive measures: Strict hemostasis, avoid contusion of the tail of the pancreas when dealing with the splenic pedicle, routinely place effective drainage under the diaphragm after operation, and timely drain the accumulated blood in the splenic fossa, all of which are effective measures to prevent subdiaphragmatic abscess.
Thrombo-embolic complications
Once it occurs in some parts of the blood vessels, such as retinal artery, mesenteric vein, portal vein trunk, etc., it will cause serious consequences. The occurrence of this complication is related to the rapid increase in platelet count after splenectomy.
Preventive measures: most of them advocate the application of anticoagulants such as heparin for preventive treatment when the platelet count exceeds 1000~2000*10⁹/L after splenectomy. If thromboembolic complications occur, anticoagulant therapy should be used, and treatment and rest, aspirin, dipyridamole and other drugs can also be added.
Postoperative precautions:
1. Observe the drainage tube and drainage volume, and routinely measure changes in blood pressure, pulse and hemoglobin. Observe the condition of the drainage tube in the subdiaphragmatic splenic fossa. If there is a tendency of internal bleeding, blood transfusion and fluid replacement should be performed in time. If the bleeding is indeed persistent, reoperation should be considered to stop the bleeding.
2. Splenectomy greatly stimulates the abdominal organs (especially the stomach), so resume eating 2 to 3 days after the operation.
3. Many patients undergoing splenectomy have poor liver function. Sufficient vitamins, glucose, etc. should be supplemented after surgery. If hepatic coma is suspected, corresponding preventive measures should be taken in time.
4. Pay attention to changes in kidney function and urine output, and be alert to the occurrence of hepatorenal syndrome.
5. Routine application of antibiotics after surgery to prevent systemic and subdiaphragmatic infections.
6. Measure the platelet count in time. If the platelet count rises rapidly to more than 50×109/L, splenic vein thrombosis may occur. If severe abdominal pain and bloody stool appear again, it indicates that the thrombus has spread to the superior mesenteric vein. Antibiotics should be used in time. Coagulation therapy, surgery if necessary.
Postoperative Diet:
1. The diet is generally started after 2-3 days after the recovery of gastrointestinal function. The initial stage is mainly liquid, and gradually transition to semi-liquid and soft food. Avoid eating irritating food and hard food.
2. To meet the protein supply, often eat lean meat, eggs, chicken, fish, dairy products, and some soybean products every day.
3. It is necessary to supply more iron-containing foods than usual to meet the needs of hematopoiesis and prevent anemia, such as animal liver, blood, lean meat, eggs, and colored vegetables.
4. Provide a variety of vitamins, eat more vegetables, fruits, eggs, milk, and maintain the intake of green vegetables and fruits every day.
Adequate sleep and a regular life should be maintained after the operation.
- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- 【4K Basics】4K Ultra HD Endoscope Camera System
- 【General Surgery Laparoscopy】"Two-step stratified method" operation flow of left lateral hepatic lobectomy
- 【General Surgery Laparoscopy】Left Hepatectomy