[Laparoscopy in Hepatobiliary Surgery] Fenestration of hepatic cyst
Release time: 06 Jun 2023 Author:Shrek
Hepatic cysts: All vesicular lesions that grow on the liver are collectively called hepatic cysts. Hepatic cyst is a relatively common benign liver disease, which can be divided into parasitic, non-parasitic and congenital hereditary. Small hepatic cysts without symptoms do not need special treatment; large hepatic cysts (generally more than 5cm) with symptoms should be treated. Common methods: 1. Cyst puncture and aspiration under the guidance of B-ultrasound. 2. Surgical "fenestration" or "roofing" of hepatic cysts, that is, part of the cyst wall is removed under laparotomy or laparoscopy, and the cyst cavity is opened to the abdominal cavity after the cyst fluid is exhausted.

Indications
1. Symptomatic hepatic cysts (non-parasitic and non-malignant)
2. Located on the surface of the liver
3. No communication with the bile duct
4. Single or multiple hepatic cysts
5. Sudden increase in cyst size (> 10 cm)
Why do you get liver cysts?
There are many causes of liver cysts, which can be divided into parasitic and non-parasitic.
Parasitic liver cysts are mainly caused by infection with parasites, and the common way is to infect the human body through raw fish, raw shrimp and other foods.
Non-parasitic hepatic cysts are affected by a variety of factors, such as inflammation, trauma, congenital factors, etc. The most common is congenital hepatic cysts, which are generally caused by abnormal development of intrahepatic bile ducts or lymphatic vessels during the embryonic period.
Do liver cysts require surgery?
Most liver cysts do not require treatment.
Hepatic cysts are common benign space-occupying lesions in the liver. Smaller hepatic cysts or asymptomatic hepatic cysts do not require surgery.
Moreover, the liver cyst itself is not very harmful. Most patients have no symptoms and basically have no impact on health. At this time, the routine practice is to regularly review and observe the changes of the lesion.
Need surgery
When the diameter of the liver cyst is greater than 10 cm, the liver cyst is accompanied by infection, which leads to painful symptoms, and the liver cyst is huge and causes the organs around the liver cyst to be compressed, such as compression of the stomach and intestines, which may cause some dyspepsia. When a liver cyst ruptures, surgery may be required.
Other cases
If it is multiple cysts in the liver, it is necessary to further look at the test results and decide on the next treatment method. If there is no discomfort and the liver cyst is relatively small, it can generally be reviewed regularly.
Surgical steps
1. Position and trocar position: The patient is in the same position as the supine position
Surgeon between the patient's legs. A 10mm trocar is placed through the subumbilical incision. Then maintain a pressure-controlled CO2 insufflation at 12-14mmHg, and continuously monitor the end-tidal CO2 concentration. Through this port, a 30° laparoscope was introduced to examine the entire abdominal viscera and determine the location of the lesion. Then, depending on their location, two additional trocars are inserted at the appropriate sites. When the surgeon punctures the abdominal wall, ensure the sharp point of the trocar in case of abdominal or retroperitoneal organ injury.
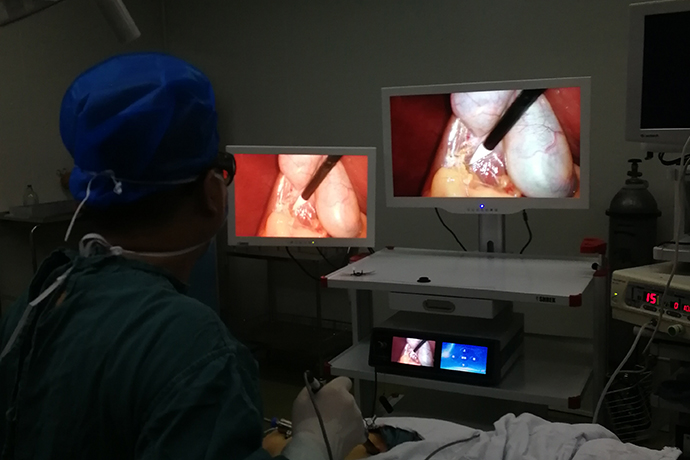
2. Laparoscopy and intervention: Introduce laparoscopy to further determine the lesion location, quantity, and interface relationship between the liver and the cyst. When the lesion is determined to be a simple hepatic cyst, we usually cut a 5 mm hole in the cyst wall using monopolar coagulation or ultrasonic dissector. A suction tube is then used to aspirate fluid from the cyst. When necessary, laparoscopic fluid collection with a needle is recommended first to determine fluid quality (bile, mucus). If the lesion is suspected to be a non-simple cyst before surgery, the intracystic fluid should be examined pathologically, bacteriologically, and biochemically.
3. Fenestration of the cystic cavity: the cavity is filled with monopolar electrocoagulation forceps, ultrasonic dissector or Ligasure. The suction cup is positioned to pick up residual liquid. After the above procedure, careful observation of the cyst wall is required. If there are thicker vessels in the wall, it is recommended to occlude the bile duct proximal to these vessels to avoid bile leakage. The goal of the surgery is adequate fenestration so that resection of the liver along the line of the lesion is not critical. For polycystic liver disease, it should be from external to internal lesions. In essence, there is no need to deal with the residual cystic cavity. However, considering that postoperative adhesions may lead to fenestration atresia, especially in polycystic liver disease and cysts near the diaphragm, the secretory epithelium in the residual cavity should be destroyed with ethanol or argon knife.
4. Drainage: When all cysts are removed, there is no bleeding and bile leakage. The drainage tube is placed in the cystic cavity. Additional piping is available if required. Insufflation is then stopped and the trocar is withdrawn. All trocar insertion sites should be carefully closed.
Hepatic cyst is a relatively common benign liver disease, which can be divided into parasitic and non-parasitic, and non-parasitic hepatic cyst is divided into congenital, traumatic, inflammatory, and neoplastic. Asymptomatic congenital hepatic cysts are very common and often multiple, more often in middle-aged women, often accompanied by polycystic kidney disease. The cystic fluid of congenital hepatic cysts is mostly colorless or transparent, and it can be brown in those with hemorrhage. Multiple cysts are often small and spread all over the liver.
- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- 【4K Basics】4K Ultra HD Endoscope Camera System
- 【General Surgery Laparoscopy】"Two-step stratified method" operation flow of left lateral hepatic lobectomy
- 【General Surgery Laparoscopy】Left Hepatectomy