[General Surgery Laparoscopy] 4K ultra-high definition laparoscopic deroofing and decompression of renal cysts
Release time: 02 Jul 2024 Author:Shrek
Simple renal cyst or acquired renal cyst is a common kidney disease, accounting for about 1/4 of adults. Its pathogenesis has not been fully elucidated. It is often isolated and unilateral. It is more common in men and mostly protrudes from the surface of the kidney. However, It can also be located in the deep cortex or medulla. If it is located in the renal pelvis or renal sinus, it is called a parapelvic cyst.
Clinical manifestations: Most patients have no clinical symptoms. When the cyst compresses the kidneys, high blood pressure, low back pain, hydronephrosis and other symptoms may occur in the renal pelvis. If infection and bleeding are caused, symptoms such as fever, waist pain, and hematuria may occur.
Diagnosis: Ultrasound examination is the preferred examination method, and CT, MRI, and cyst puncture and cyst fluid examination are used to further identify malignant transformation and other lesions.
Treatment methods: Those with a diameter less than 5cm, no obvious renal parenchyma, compression of the renal pelvis, and no infection, malignancy, or hypertension only need regular reexamination; those with a diameter greater than 5cm, or even though it does not reach 5cm, compresses the renal pelvis and causes hydronephrosis, and it is confirmed that the cyst wall has Malignant transformation requires surgical treatment. Laparoscopic deroofing and decompression of renal cysts is currently the gold standard for surgical treatment. When the cyst is severely infected or compresses the kidney, causing severe damage to renal function or malignant transformation, the diseased kidney must be removed.
Key points and experience of surgery
1. Posture
The "jackknife position" is the most commonly used surgical position, following the traditional open posterior approach surgical position. The advantage is that it is easy to place the trocar, but the disadvantage is that the operator's visual axis, operating axis and center of gravity are separated, and the operator will easily become fatigued if it takes too long. The "Guo's body position" improved by Academician Guo Yinglu can avoid these shortcomings. The key points are: the head is as far forward as possible, the hips are as far back as possible, the waist is facing the waist bridge, and the body is vertical to the ground.
2.Trocar placement
Generally, it is 2cm above the highest point of the iliac spine. The operating holes for the left and right hands are located in the front axillary line and 1-2cm below the tip of the 12th rib. The three holes are best in an isosceles triangle. The distance is about 1 punch. They can be moved appropriately according to the surgical area and the height of the patient. and waist width adjustment, but cannot mechanically memorize several anatomical landmark points.
3. Establish the retroperitoneal cavity
There are mainly "scope method" and "balloon dilation method".
The "scope method" is to use the scope to expand the retroperitoneal space after the observation hole trocar enters the extraperitoneal fat layer and connects to the pneumoperitoneum expansion. The difficulty lies in the trocar's control of the puncture depth. The general principle is the same as percutaneous nephroscopic puncture. , it is better to be shallow rather than deep, you can try it many times until you can see the "cobweb-like" tissue under the muscle, then use the bevel of the lens close to the top wall, and use the other hand close to the skin to feel and guide the movement of the lens, you can have " "Fiber stripping sensation", after skilled operation, the retroperitoneal space can be expanded at one time, the long needle is positioned at the puncture point and then the trocar is inserted with left and right hands.
The "air bag expansion method" is divided into homemade air bags and finished air bags. The steps are to take 1-2cm below the tip of the 12th rib, incise the skin 2-3cm, use large curved forceps to break through the deep external oblique aponeurosis and expand it. Generally, there are two layers. "Breakthrough feeling", then the index finger enters the extraperitoneal fat space along the incision to separate it, and a balloon is inserted to expand it. Generally, the depression of the iliac spine is full.
Establishing the retroperitoneal cavity is the most critical step. Failure to establish the retroperitoneal cavity means failure of retroperitoneal surgery, which has also become a "stumbling block" for beginners. There is no difference between the "scope method" and the "balloon dilatation method". They are both inferior and can complement each other. When the "scope method" fails, the "balloon dilation method" can be used instead. When the "balloon dilatation method" fails, the "scope method" can also be tried.
Relatively speaking, the "scope method" is more suitable for retroperitoneal laparoscopic renal cyst deropping because the incision is smaller. If the surgeon is confident, only 5mm trocar can be placed in the operating hole of the left and right hands, and only one stitch is needed after the operation. . Of course, you can master both methods best, and only the one you are familiar with is the most suitable.
4. Free extraperitoneal fat
It is the most easily overlooked step. Many people think that cleaning fat is a waste of time. However, separation and hemostasis must be used when cleaning fat. It is also the "basic exercise" of laparoscopy and is a rare practical opportunity for beginners.
First, we need to find the avascular layer between the extraperitoneal fat and Gerota's fascia. The fat is generally visible from the bottom (see video for details). Obese patients should not be impatient to prevent the layer from being too deep to damage the peritoneum and other tissues and organs. And downward, move clockwise or counterclockwise, paying special attention to the position of the iliac fossa. Due to the limited operating space, it is easy to lose the level.
After freeing the fat, for the "air bag method", you can directly use oval forceps to clamp large pieces of fat. For the "scope method," you can use "spoon forceps" to clean the fat. You can also use scissors to cut the fat into small pieces and suction with a suction device. There are also innovative methods by the surgeon. Use a prostate breaker to clean out fat.
5. Look for cysts
The Gerota fascia is incised close to the psoas major muscle, and the dorsal side of the kidney is freed along the retrorenal space between the psoas major muscle and the perinephric fat sac, and the ventral side of the kidney is freed along the prerenal space between the peritoneum and the perinephric fat sac. The prerenal space and the retrorenal space are relatively avascular. When encountering fat nutrient vessels, the bleeding can be pre-stopped and then severed. Then the renal fat sac is incised, the cyst is found based on the preoperative CT positioning, and the cyst is completely removed about 5mm away from the renal parenchyma. The cyst wall can be rubbed with iodine or the residual cyst wall can be sutured to reduce the chance of cyst recurrence.
Surgery cases
1. Case introduction: The patient was a 60-year-old male who came to the hospital mainly because of "a cyst in the right kidney was found on physical examination and ultrasound for 1 month." B-ultrasound showed an echoless area in the right kidney, approximately 8.4cm × 7.8cm in size, with clear borders. In the past, he had old cerebral infarction, multiple liver cysts, emphysema, and pulmonary bullae. The diagnosis was a right renal cyst. Retroperitoneal laparoscopic deropping of the right renal cyst was performed.
2. Enhanced CT of the urinary tract showed a round low-density shadow in the right kidney, with a diameter of 8.1cm×7.1cm×5.0cm. A small amount of calcification could be seen in the wall. There was no enhancement on the enhanced scan. No contrast agent was seen during the excretion phase. The right kidney should be considered for diagnosis. Renal cyst.
3. Enhanced CT sagittal view shows that the cyst is located slightly dorsally on the upper pole of the right kidney.
4. Enhanced CT coronal view shows that the cyst is located lateral to the upper pole of the right kidney.
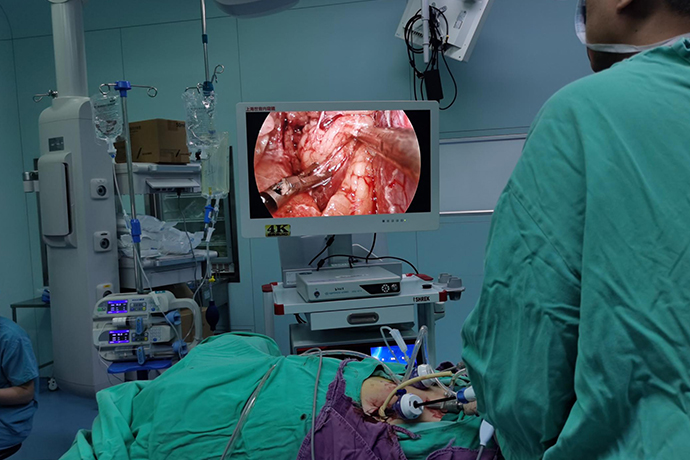
5. For retroperitoneal surgery, extraperitoneal fat is first freed. The lateral vertebral fascia is incised, the dorsal level of the kidney is freed, and the ventral level of the kidney is moderately freed. The renal fat sac was incised along the ventrodorsal junction along the long axis of the kidney and dissociated to the level of the renal capsule.
6. Incise the renal fat sac from the foot side to the head side, and encounter the renal cyst in the upper pole of the kidney. There is a capsule rich in small blood vessels on the surface of the cyst, and this capsule needs to be incised during the operation to enter the correct layer. Correctly layered renal cysts have a bluish surface and no small blood vessels on the surface.
7. There is usually a layer of white loose connective tissue between the renal fat sac and the renal cyst. The ultrasonic knife edge of the right hand is closed, and the blunt dissociation effect of the ultrasonic knife rod is used to separate this layer of loose connective tissue. This blunt dissociation technique is like stroking the cheek. It can not only achieve blunt dissociation, but also avoid excessive compression and damage to the renal cyst.
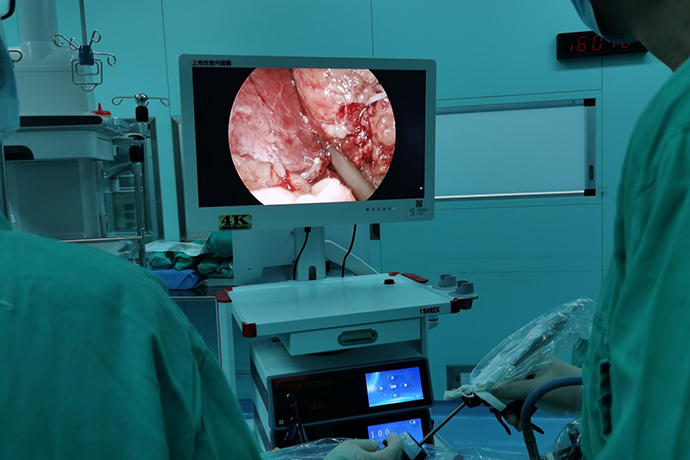
8. The procedure of puncturing the renal cyst and aspirating the cyst fluid tests the operator's hands-on coordination ability. The puncture position of the ultrasonic scalpel should be at a higher position facing the right hand.
9. At the moment when the metal rod of the ultrasonic scalpel pierces the renal cyst, the left-hand suction rod is quickly inserted into the cyst through the breach to suck out the cyst fluid. Avoid extravasation of cyst fluid causing edema of surrounding tissues.
10. After the cyst fluid is sucked out by the suction device, the cyst wall collapses, exposing a new operating space. The left hand curved forceps are used to clamp the collapsed cyst, and the right hand ultrasonic scalpel continues to separate and expose the ventral side of the cyst, free the renal fat sac, and expose the renal parenchyma.
11. Make an incision at the junction of the cyst wall and the renal parenchyma (slightly toward the side of the cyst), leaving a small edge of the cyst wall for the renal parenchyma. Avoid renal parenchymal damage and bleeding. When using the curved forceps of the left hand to pull the cyst wall, the angle needs to be changed to facilitate direct vision and facilitate cutting with the right hand. After the resection is complete, bipolar electrocoagulation can be used to stop bleeding at the edges. When applying bipolar electrocoagulation, it is necessary to ensure that the two clamps of the bipolar device are "bluffed" apart and not too tight to "clamp". This can not only ensure the safe application of the device, but also ensure the hemostatic effect.
12. The concave surface of the kidney of the cyst should be avoided as much as possible. Once the concave surface of the cystic kidney is damaged, even if bipolar electrocoagulation is used to stop bleeding, the hemostatic effect is poor and stubborn bleeding is likely to occur.
13. At the end of the operation, the free extraperitoneal fat needs to be put into a specimen bag and taken out of the body. The removal of extraperitoneal fat is an easily missed step after surgery. First, insert the specimen bag into the retro-abdominal space through the puncture device. The bottom of the specimen bag is close to the head side, and the mouth of the specimen bag is close to the foot side, in an "inverted shape". The two curved pliers of the left and right hands cooperate with each other to unfold the shrunken specimen bag. Clamp the retroperitoneal fat close to the back side of the specimen bag opening, turn and roll the fat mass toward the inside of the specimen bag until it completely enters the specimen bag. Tighten the shrink line at the mouth of the specimen bag to complete the bagging process.
The patient's recovery from the incision after surgery, with minimal trauma.
- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- 【4K Basics】4K Ultra HD Endoscope Camera System
- 【General Surgery Laparoscopy】"Two-step stratified method" operation flow of left lateral hepatic lobectomy
- 【General Surgery Laparoscopy】Left Hepatectomy