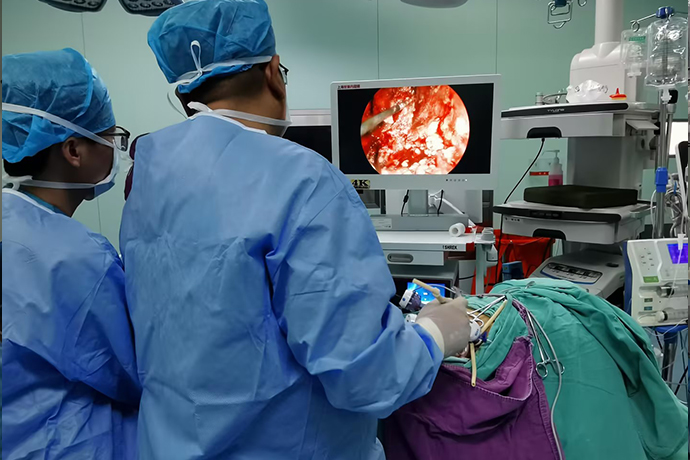
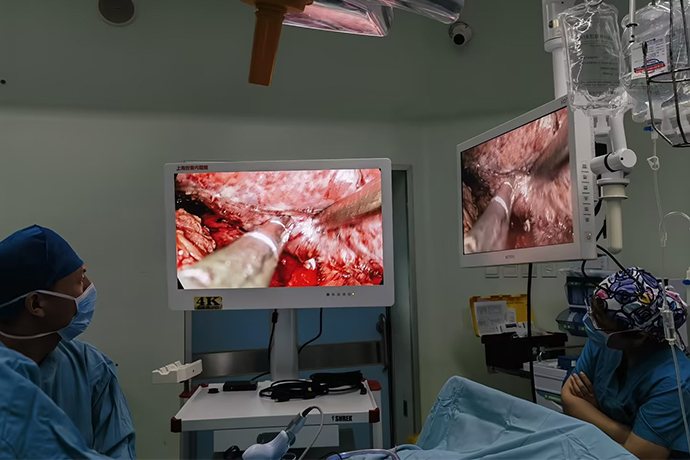
[Laparoscopy of Hepatobiliary Surgery] Common bile duct stone surgery
Release time: 24 Sep 2024 Author:Shrek
With the increasingly widespread application of minimally invasive surgery in abdominal surgery, the popularization of laparoscopic technology, the increasing experience of general surgeons, and the continuous improvement of laparoscopic skills, laparoscopic combined choledochoscopy cholecystectomy + common bile duct incision and stone removal (LC +LCBDE) has become an effective means of treating common bile duct stones.
Indications
The ideal indication for LCBDE should simultaneously meet the following four conditions:
1. Common bile duct stones: gallbladder stones complicated by secondary common bile duct stones (LC+LCBDE), or primary common bile duct stones; primary extrahepatic and extrahepatic bile duct stones without bile duct stenosis, the stone can be removed through choledochoscopy without the need for gallbladder or intestinal gallbladder removal Drainage; or common bile duct stones combined with obstructive jaundice or acute cholangitis.
2. Common bile duct diameter>1.0cm.
3. The stones in the common bile duct may be single or several.
4. Common bile duct stones <1.5cm.
Contraindications
1. For patients with primary intrahepatic bile duct stones, it is difficult to remove the stones through choledochoscopy or liver resection is required. 2. The lower end of the common bile duct is stenotic and requires cholangiojejunostomy.
3. The diameter of the common bile duct is <1.0cm, and laparoscopic common bile duct incision may cause serious side injuries and postoperative bile duct stenosis.
4. If the common bile duct stone is too large, it will be difficult to remove the stone with a stone extraction net.
5. Severe adhesions in the abdominal cavity, especially in the porta hepatis, made it impossible to dissect and expose the common bile duct.
6. Other contraindications to open surgery (various conditions that cannot be treated by surgery, such as severe cardiopulmonary insufficiency, coagulation mechanism disorders, etc.).
Technical advantages
Laparoscopic combined with fiberoptic choledochoscopy through cystic duct common bile duct exploration and lithotomy (LTCBDE) does not require dissection of the common bile duct, does not damage the physiological structure of the common bile duct, is less invasive, does not require the placement of T-tubes and suturing of the common bile duct, and the long-term T-tube indwelling This leads to a greatly increased risk of electrolyte imbalance and accidental tube removal, which brings inconvenience to patients' lives. The effect of T-tube-free surgery is significantly better than that of T-tube drainage, and it significantly reduces the incidence of bile leakage, bile duct stenosis and obstruction. It can effectively avoid the inconvenience caused by indwelling T-tubes, shorten the postoperative hospitalization time, and reduce hospitalization fees. It can greatly reduce the patient's pain and economic pressure. It fully reflects the superiority of this surgical procedure and is very obvious in suitable cases.
1. Body wall neuromuscular protection from severing.
2. There is little organ interference and quick recovery after surgery.
3. The puncture port is flexible and convenient for continuous treatment of multiple diseases.
4. The threat of infectious diseases is small and surgical personnel are safer.
Item preparation
1. Instruments: laparoscope, pneumoperitoneum, choledochoscope.
2. Instruments: endoscopic bag, surgical endoscopic instruments, debridement bowl, and dry cylinder. to
3. Dressings and disposable supplies: general external dressing, clothing bag, large hole drape, 3-0 silk thread, 5ml syringe, gloves, suction device connecting tube, beauty compress, 4-0 absorbable thread, debridement trocar, 11 #Blades, electron microscope covers, various types of T-tubes and drainage bags, and latex tubes.
Position: Lying on your back with your head high and feet low, tilting 15º-30º to the left side.
Anesthesia method: general anesthesia.
Operation steps
1. Perform routine skin disinfection and draping. Arrange the endoscopic instruments on the sterile instrument table in the order of use: hand over toothed oval forceps and three pieces of iodophor gauze to disinfect the skin; assist the doctor in laying out sterile drape. Pass a small gauze pad with alcohol to disinfect the skin. The nurse who washes her hands passes the trachea, suction tube, cold light source line, monopolar line, and the electron microscope cover to the lens; the circulating nurse connects the cold light source line, lens line, infessor machine, television system, monopolar line, and suction tube, and The footrest is placed on the side of the surgeon's feet.
2. Establish pneumoperitoneum. Make a 10mm arc incision on the upper or lower edge of the umbilicus, and puncture the abdominal wall with the Veress needle. After confirming that the Veress needle has entered the abdominal cavity, connect the CO2 pneumoperitoneum machine and start the surgical operation after reaching the pneumoperitoneum pressure: pass the No. 11 blade on the umbilicus Make a 10mm arc incision on the upper or lower edge, use 2 towel forceps to lift the abdominal walls on both sides of the umbilical fossa, pass the Veress needle to the surgeon for puncture, and use a needleless 5ml syringe filled with normal saline to connect to the Veress needle. After confirming that the Veress needle has entered the abdominal cavity, connect the CO2 Veress machine until the predetermined Veress pressure (1.73-2.00kpa) is reached and then remove the Veress needle.
3. Place a Trocar and observe the abdominal cavity, gallbladder and common bile duct: insert a 10mm Trocar through the incision, insert a telescope into the cannula for observation, and place it sequentially 3cm below the xiphoid process in the midline of the upper abdomen, 3cm below the right costal margin at the right midclavicular line, and in the right anterior axillary line. With the corresponding Trocar placed under the costal margin, the circulating nurse can place the patient in a head-to-foot position and tilt the patient 30º to the left to facilitate the surgeon's operation.
4. Dissect the gallbladder triangle, process the cystic duct and cystic artery, and fully expose the common bile duct: use toothed grasping forceps to clamp the bottom of the gallbladder, electrocoagulation separation hooks to free the cystic duct and cystic artery, and use titanium clamps at the proximal end of the cystic duct. One titanium clip was applied to each end of the cystic artery and the distal end, and two titanium clips were applied to the proximal end of the cystic artery. Absorbable titanium or nylon clips are also available. Fully dissect to expose the common bile duct.
5. Confirm and cut the common bile duct: Pass a No. 7 needle to puncture and extract the bile. After confirming that it is the common bile duct, place a piece of gauze at the omental hole to prevent bile and stones from leaking into the small omental sac. Use scissors to cut the common bile duct lengthwise. 8-10mm.
6. Exploration of the common bile duct and removal of stones: Remove the stones with stone forceps or squeeze out the stones with forceps. Then, under the supervision of the laparoscope, insert a choledochoscope through the 10mm Trocar puncture hole under the xiphoid process to explore the common bile duct and remove the stones with a basket. Remove the stones at any time. Put it into the specimen bag to prevent the stones from being lost, and flush the common bile duct after removing the stones.
7. Place a T-tube for drainage: select a suitable T-tube, trim it and insert it through a hole under the xiphoid process. Use a separation forceps to insert the two short arms into the common bile duct, and hold the needle with a 4-0 absorbable needle. The common bile duct was sutured with interrupted threads, and then the T tube was led out of the body through the 5mm Trocar puncture in the midclavicular line under the right subcostal margin, and 50 ml of normal saline was injected into the cavity to observe whether there was leakage around the suture of the common bile duct.
8. Remove the gallbladder and treat the wound on the liver bed: use electrocoagulation to cut off the cystic duct and cystic artery, use grasping forceps and electrocoagulation separation hook to separate the gallbladder bed, place the gallbladder on the upper right side of the liver, and use electrocoagulation rod to carefully stop bleeding on the liver bed. , connect the flushing and suction device to warm saline flushing and check for active bleeding and bile leakage, and return the operating bed to a horizontal position.
9. Remove the gallbladder: Clamp the neck of the gallbladder with the grasping forceps, and lift it out together with the puncture cannula through the umbilical incision or subxiphoid incision. Use the curved vascular forceps, suction head, and scissors for backup.
10. Check whether there is blood and fluid in the abdominal cavity, then pull out the laparoscope, open the valve of the cannula to remove the CO2 gas in the abdominal cavity, and suture the wound: For those who need abdominal drainage, drain it from the 5mm Trocar puncture in the front axillary line under the right costal margin. Use a 10X28 angle needle and 3-0 silk thread to suture each incision and cover the wound.
Postoperative drainage management
1. Abdominal drainage tube management
Properly fix the drainage tube externally to avoid distortion or pressure, maintain smooth drainage of the abdominal drainage tube, and observe the drainage volume and characteristics. Generally, the abdominal drainage tube is removed 48-72 hours after surgery. If the drainage volume is large or bile fluid is introduced, the time of removing the tube must be delayed.
2. T-shaped tube management
(1) Properly fix the T-shaped tube outside the body to maintain smooth drainage. If the T-shaped tube has poor drainage and squeezes the T-shaped tube, the rubber tube will automatically expand and generate negative pressure, which will block the T-shaped tube with stone residues, inflammatory secretions, etc. Aspirate out. If necessary, use 5-10ml saline to gently flush the T-tube and withdraw bile.
(2) Observe the amount of drainage every day. Due to the influence of anesthesia after surgery, the amount of bile secretion is less. After the diet is resumed, the amount of bile can increase by 500 to 800ml. If more than 2000ml of thin bile is produced every day, it indicates poor liver function, and it is necessary to protect the liver and pay attention to replenishing water and electrolytes.
(3) Elevate the T-shaped tube or intermittently clamp the T-shaped tube one week after the operation to allow bile to flow into the intestine to avoid excessive bile loss.
(4) T-tube angiography 10 to 12 days after surgery. If there are no residual stones and the lower end of the common bile duct is unobstructed, the tube can be clamped and discharged the day after the angiography. After discharge, the T-tube can be flushed with 100-200ml of metronidazole solution 1-1 times a week. 2 times, loosen the clamp for 2-3 hours every day to allow bile to flush the T-shaped tube and prevent bacterial growth in the tube.
(5) For patients with jaundice, T-shaped tube drainage can help the jaundice subside and the tube clamping time can be relatively delayed. If jaundice subsides slowly and major biliary obstruction is ruled out, capillary cholangitis and capillary hepatitis should be considered, and hepatoprotective, hormone, and hyperbaric oxygen therapy can be adopted.
(6) The time to remove the T-tube: Laparoscopic surgery is less invasive, and it takes longer to form a solid sinus around the T-tube than open surgery. Therefore, the time to remove the T-tube should be 1-2 months after surgery. If postoperative biliary examination is required, And stone removal is safer after 2 months after surgery.
Complications and treatment
Complications of LC surgery can also occur in patients undergoing LCBDE surgery and require great attention. LCBDE can also cause the following complications:
l. T-shaped tube prolapse
The prolapse of the T-shaped tube is mostly due to accidental factors. It can also be caused by placing the T-shaped tube too straight in the abdominal cavity. Postoperative abdominal distension or coughing can cause the T-shaped tube to prolapse outside the bile duct, causing bile leakage. The shorter the time between T-tube prolapse and surgery, the greater the severity. If the sinus tract is not completely formed within 5-7 days, bile leaks and accumulates in the subhepatic space after T-tube prolapse, or bile peritonitis occurs. It is advisable to perform laparoscopic or laparotomy surgery as soon as possible to reset the T-shaped tube and fully drain the abdominal cavity; 7-10 The sinus tract in Tianhou has been completely formed and the T-shaped tube has prolapsed. As long as the sinus tract is not ruptured, the drainage of the fistula is maintained and conservative treatment is performed under close observation. Generally, there will be no serious consequences. If the sinus tract is not firm and ruptures, peritonitis or bile accumulation occurs, it is advisable to prescribe treatment. Abdominal surgery.
2. Bile leakage and biliary peritonitis after extubation
In clinical practice, regardless of open or laparoscopic surgery, bile leakage and bile peritonitis have been reported after T-tube removal within 1 to 2 months after surgery. The factors may be many:
①The patient's nutritional status is poor, frail and emaciated, etc.
② There is a history of omentectomy, or the omentum has been adhered to other parts of the abdominal cavity.
③ Improper extubation method after surgery, such as excessive force causing sinus rupture.
Correct method to remove T-tube:
① Open the T-tube to drain bile for more than half an hour before extubation.
② Before extubation, instruct the patient to cough vigorously to expel bile from the biliary tract as much as possible to avoid high blood pressure in the biliary tract.
③When extubating the tube, press the abdominal wall of the T-shaped tube with one hand and slowly pull out the T-shaped tube with force to avoid pulling or rupturing the fibrous tissue sinus formed by the T-shaped tube in the abdominal cavity.
④After extubation, lie down and rest for 1-2 hours.
Bile leakage caused by removal of the T-tube can generally be cured conservatively without the need for surgery only by promptly re-inserting the tube for unobstructed drainage and taking anti-infective treatment.
Complications and prevention
Laparoscopic bile duct exploration and cholecystectomy are also potentially dangerous. If not handled properly, they can cause a variety of serious complications, including:
1. Intraoperative and postoperative bleeding. The key to prevention and treatment lies in strict control of the location of common bile duct incision and precise operation during surgery.
2. Bile leakage. The key to prevention and treatment: avoid damage to the common bile duct and use sophisticated techniques to suture the common bile duct.
3. Biliary stricture. The key to prevention and treatment: Strictly grasp the indications, accurately suture the common bile duct, and prevent thermal damage to the bile duct.
4. Residual stones in the bile duct. The key to prevention and treatment: remove all stones during surgery, perform angiography before removing the T-tube after surgery, and use choledochoscope to remove stones from the common bile duct through the T-tube.
5. Abdominal infection. Key points of prevention and treatment: Prevent bile from overflowing or leaking into the abdominal cavity, place abdominal drainage, and fight infection after surgery.
6. Injury to other internal organs. Key points of prevention and treatment: careful operation.
7. Complications related to pneumoperitoneum. Preventive measures: Appropriate intraperitoneal air pressure, and deflate the pneumoperitoneum at the end of the operation.
As technical proficiency increases, the incidence of the above complications becomes significantly lower.
Any technology has its own rationality and inherent limitations, and must be selected and applied based on the patient's specific situation in order to achieve the most ideal effect.
- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- 【4K Basics】4K Ultra HD Endoscope Camera System
- 【General Surgery Laparoscopy】"Two-step stratified method" operation flow of left lateral hepatic lobectomy
- 【General Surgery Laparoscopy】Left Hepatectomy