【Hepatobiliary Surgery Laparoscopy】Splenic Tumor Surgery
Release time: 08 Oct 2024 Author:Shrek
The spleen is an important lymphoid organ in the human body. It is located under the diaphragm and is protected by the surrounding bones. Therefore, the early symptoms of spleen tumors are not obvious and are not easily discovered by people, thus delaying the treatment of the disease. The symptoms of splenic tumors are related to the nature, location, size and degree of splenomegaly of the tumor. Common clinical symptoms include:

Clinical symptoms
1. Splenomegaly is mostly accompanied by left upper quadrant discomfort, pain and compression symptoms, such as abdominal distension, nausea, constipation, dyspnea, etc.
2. There is a certain relationship between hypersplenism and splenomegaly, but the symptoms are not proportional to the degree of splenomegaly. For unexplained hypersplenism accompanied by splenomegaly, the presence of tumors, especially hemangioma, should be highly suspected.
3. Systemic symptoms are more common in malignant tumors of the spleen, manifesting as low-grade fever, anemia, fatigue, general discomfort, weight loss, cachexia, etc.
4. Spontaneous rupture of splenic tumors is rare clinically and manifests as sudden abdominal pain, peritonitis, and may lead to hemorrhagic shock or even death. If splenic rupture is accompanied by early metastasis, it is the worst prognostic factor. Spontaneous splenic rupture may be secondary to hemophagocytic syndrome, hemangiopericytoma and serosal multiple hemangioma, T-cell leukemia, etc. Some cases may be accompanied by intraperitoneal implantation metastasis, which is more common in spontaneous rupture of splenic hemangioma and angiosarcoma.
Splenic tumors are very rare, and benign tumors are more common than malignant ones.
Benign hemangiomas are the most common (50%), followed by lymphangiomas, hamartomas, etc.
Malignant lymphoma is the most common malignant tumor (70%~80%), followed by metastases, angiosarcoma, fibrous histiocytic sarcoma, etc.
The CT features of splenic tumors are relatively unobvious, so the diagnosis should be based on comparison.
Disease classification
The classification of splenic tumors is relatively complex and is divided into the following five types according to the source of tissue components: (1) Tumor-like lesions: including non-parasitic cysts and hamartomas. (2) Vascular tumors: divided into benign and malignant. (3) Lymphoid tumors: Hodgkin's disease, non-Hodgkin's disease, lymphoid lesions. (4) Non-lymphoid tumors: including lipoma, malignant fibrocytoma, malignant teratoma, etc. (5) Tumor-like lesions: such as traumatic cystic pseudotumor, inflammatory pseudotumor, etc. Spleen tumors are more benign than malignant. Among benign tumors, splenic cysts are the most common, and malignant lymphomas are more common among malignant tumors.
Splenic tumors are divided into the following types according to their origin: (1) Vascular origin. (2) Source of lymphoid tissue. (3) Origin of embryonic tissue. (4) Source of nervous tissue. (5) Other sources of mesenchymal tissue: such as fibrous tissue, adipose tissue and smooth muscle tissue.
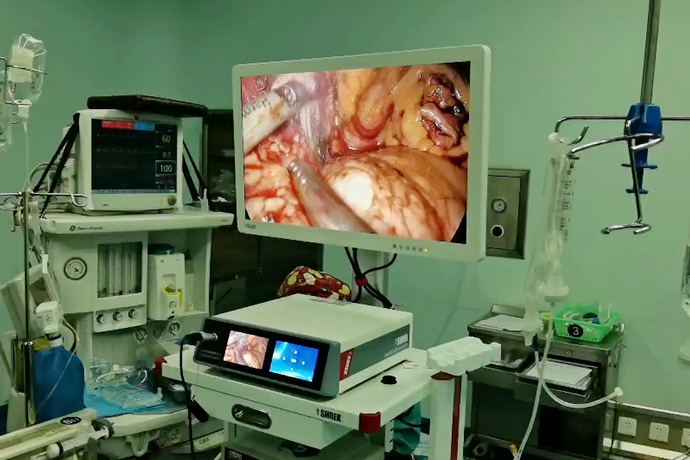
Surgical procedure
Position: After the patient is under general anesthesia, he should lie on his right side at 40° with the head elevated at 30°, so that the greater omentum, stomach and colon can be moved away from the spleen under the action of gravity and obtain a good surgical field of view.
A 10 mm incision was made at the upper edge of the umbilicus and pneumoperitoneum was established. The pneumoperitoneum pressure was maintained at 14 mmHg. A 30° laparoscope was inserted to explore the abdominal cavity.
The position of the cannula: Insert a 12 mm cannula at the left midclavicular line, 2 cm below the spleen, as the main operating hole (for the surgeon to use ultrasonic scalpel, Ligasure and linear cutting closure device); place a 5 mm cannula under the xiphoid process The tube is used as an auxiliary operating hole (for the operator to use grasping forceps); a 5 mm trocar is placed 2 cm below the spleen in the left anterior axillary line as an auxiliary operating hole (for the first assistant to use laparoscopic grasping forceps and suction device).
Free spleen. When resecting the lower pole of the spleen, it is necessary to free the splenocolic ligament and part of the spleen and gastric ligament and splenorenal ligament. When resecting the upper pole, it is necessary to free the splephrenic ligament and the corresponding spleen and gastric ligament (the thicker short gastric blood vessels can be coagulated with Ligasure) and the spleen. Renal ligament.
To deal with the splenic hilum branch vessels, one pole of the spleen needs to be removed, and the splenic branch arteries and veins are freed toward the splenic hilum. Small blood vessels can be directly coagulated with Ligasure (<5 mm), and large blood vessels can be clamped and severed with synthetic clips. During dissection, observe the ischemic area of the spleen. If the resection range is not reached, dissection can continue to the splenic hilum (be careful not to damage the splenic artery and vein at this time) until the ischemic range reaches the intended resection range.
Partial resection of the spleen: Cut off the spleen 1 cm inside the ischemic area (ultrasound scalpel and Ligasure are used in combination), use bipolar electrocoagulation to stop bleeding, and cover the wound with hemostatic gauze. Finally, the specimen is bagged and cut into pieces, and a drainage tube is placed in the splenic fossa to complete the operation.
1. Explore the abdominal cavity, open the omental sac to the splenic hilum, and pre-treat some short gastric blood vessels.
2. Separate the pancreaticogastric ligament; suspend the greater curvature of the gastric body.
3. Separate the adhesive omentum tissue in the splenic hilum area to expose the splenic hilum.
4. Separate the adhesions of the lower pole of the spleen and the splenocolic ligament.
5. Isolate and process the lower pole blood vessels of the spleen.
6. Hold up the lower pole of the spleen and separate the lower part of the splenorenal ligament and the retrosplenic hilum space.
7. Isolate the splenic artery at the upper edge of the pancreas and ligate it with No. 7 silk suture.
8. Open the retroperitoneum on the inside of the capsule of the upper pole of the spleen above the tail of the pancreas, gradually separate the spleen and stomach fundus space upward along the direction of the fundus of the stomach, and deal with the remaining short gastric blood vessels.
9. Lift the upper pole of the spleen, separate the splenophrenic ligament and the upper part of the splenorenal ligament, and join the lower part.
10. Use a gold finger to penetrate the tunnel behind the splenic hilum and tie the splenic pedicle with No. 7 silk suture.
11. Then use gold fingers to penetrate the posterior tunnel of the splenic pedicle, and use Endo-GIA blue nails or white nails to close and separate the splenic pedicle.
12. Check the splenic pedicle stump and strengthen it with titanium clips.
13. Separate the residual splenorenal ligament.
14. The specimen is bagged and the specimen is removed through the enlarged umbilical hole.
15. Re-enter the microscope to check for bleeding from the wound, whether there is any damage to the gastric wall, and whether the closed stump is reliable.
16. Place drainage tubes in the splenic fossa and splenic pedicle section.
17. Remove the gastric suspension.
18. Remove pneumoperitoneum and suture the incision.
Postoperative pathology
Gross: 1 spleen specimen, approximately 15.0 cm × 8.2 cm × 3.0 cm in size. Part of the spleen tissue was severed. The cross-section was bean paste red. No hematoma was visible in the parenchyma. No obvious gray-white mass was found in multiple cross-sections.
Pathological diagnosis: chronic congestive splenomegaly.
Summarize
The surgery is safe and feasible for experienced minimally invasive surgeons. At the same time, laparoscopic partial splenectomy has the following advantages: low intraoperative blood loss and short operation time; fast postoperative recovery and few complications; retaining the important role of the spleen in immunity and anti-tumor; good cosmetic effect, and easy for patients to accept . In view of this, laparoscopic partial splenectomy may partially replace total splenectomy and become a new minimally invasive surgical method for the treatment of splenic diseases.
- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- 【4K Basics】4K Ultra HD Endoscope Camera System
- 【General Surgery Laparoscopy】"Two-step stratified method" operation flow of left lateral hepatic lobectomy
- 【General Surgery Laparoscopy】Left Hepatectomy