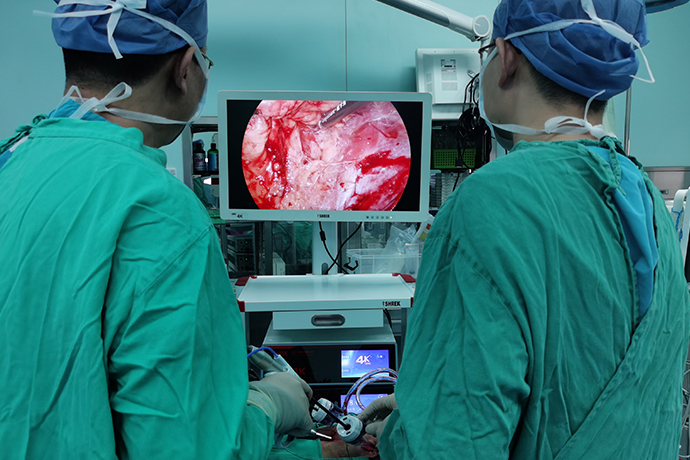
[General Surgery Laparoscopy] 4k ultra-high definition laparoscopy for prostate cancer
Release time: 04 Jun 2024 Author:Shrek
Prostate cancer is a common male disease that occurs in the male reproductive organs. It will have a certain impact on men's health and quality of life. So, what methods can be used to treat men with prostate cancer? So let’s find out. The incidence of prostate cancer is mainly middle-aged and elderly men over 50 years old, and as men age, the incidence rate of prostate cancer will also show an upward trend. But when patients suffer from prostate cancer, there are no obvious specific symptoms in the early stages. The symptoms of prostate cancer are very similar to those of benign diseases such as prostatic hyperplasia and prostatitis. If a patient has symptoms such as difficulty urinating, frequent urination, urgency, and waiting to urinate, they can easily be ignored by the patient if they are not obvious.

When prostate cancer develops to an advanced stage, patients may experience systemic symptoms such as fatigue, weight loss, and body pain. If the tumor tissue metastasizes to the bone, it will also cause bone pain at the metastasis site. However, if these systemic symptoms occur, the prognosis will be poor if treated again. Therefore, the key to the treatment of prostate cancer is early diagnosis and detection. The treatment of prostate cancer, like other malignant tumors, is a multidisciplinary and comprehensive treatment process. Clinically, surgery, radiotherapy, endocrine therapy and other methods can be used for treatment. Because the early diagnosis rate of prostate cancer is relatively high, many patients are eligible for radical surgery, and they can obtain very good prognosis after surgery. Therefore, surgical treatment is the most important, most direct, and most well-known treatment method for radical prostate cancer treatment.
Current surgical treatment methods for prostate cancer mainly include traditional laparotomy and 4k laparoscopic radical prostatectomy. Both surgeries can effectively remove cancer cells in the patient's prostate, thereby achieving a radical cure. Compared with traditional open surgery, 4k ultra-high definition laparoscopic radical prostatectomy has many unique advantages.
(1) The tumor is well controlled. 4k Laparoscopic radical prostatectomy and open surgery are equally effective in removing tumors. There is no statistical difference in the positive margin rate and tumor residual rate between 4k laparoscopic radical prostatectomy and open surgery, and the long-term postoperative survival of the two surgical methods is consistent.
(2) There is little intraoperative damage and less bleeding. According to reports, the intraoperative blood loss during 4K ultra-high-definition laparoscopic radical prostatectomy is only one-quarter of the blood loss during open surgery. This provides a good view during surgery and also reduces the risk of damage to surrounding tissue during surgery.
(3) Recovery is quick after surgery. After open surgery, patients often need to have an indwelling urinary catheter for about 15 days, while patients who undergo 4k laparoscopic radical prostatectomy can often have their urinary catheter removed about 1 week after surgery. In addition, 4k laparoscopic radical prostatectomy has significantly shortened the average length of stay for patients, reducing patients’ pain while saving medical expenses.
The pelvic fascia is opened and the deep dorsal venous complex (DVC) is addressed.
Remove fatty tissue from the surface of the prostate, bladder neck, and pelvic fascia. Press the prostate to the opposite side and incise the bilateral pelvic fascia close to the pelvic side wall (away from the prostate). The puboprostatic ligament was cut and the DVC was sutured.
Free and preserve the bladder neck
The gap between the bladder neck and the prostate is identified by pulling on the urethra. The dissection is performed along the plane between the prostate and bladder neck, extending to both sides. After the tissues on both sides of the bladder neck are completely separated, the urethral mucosa at the bladder neck can be observed, the anterior wall of the urethra is incised, and the urinary bladder is extracted and removed. Cut off the posterior lip of the bladder neck close to the prostate until the urethra at the bladder neck is completely severed.
Free seminal vesicle
The vesicoprostatic muscle (VPM) is incised from just behind the bladder neck (5 to 7 o'clock) to the level behind the seminal vesicle. Use an aspirator to bluntly separate both sides of the seminal vesicle from behind, find the vas deferens, clamp and cut off the vas deferens, and bluntly free the seminal vesicles along the direction of the vas deferens. Pay attention to the course of the seminal vesicle artery outside and below the seminal vesicle, and use ultrasonic scalpel or Hem-o-lock clamp to avoid bleeding. After the seminal vesicles on both sides are freed, the vas deferens and seminal vesicles are pulled upward together, and Diel's fascia can be observed.
Dealing with Dickinson's fascia and prostatic ligaments
The vas deferens and seminal vesicles are pulled upward to expose Dickinson's fascia. After sharp transverse incision of Dickinson's fascia, the anterior rectal space of the prostate is exposed. The prostate is closely dissected behind the prostate and bluntly dissected forward to the tip of the prostate. Pull the prostate forward to the opposite side to expose the ligaments on both sides of the prostate. If the vascular and nerve bundles are not preserved, prostatectomy can be performed at the "extrafascial" level. At this time, using energy devices such as Li-gasure or KLS to treat the prostatic ligaments on both sides can reduce bleeding. After dissociating the seminal vesicles, a fat-like structure can be observed on the side of the prostate above and outside the seminal vesicles. If the neurovascular bundle is preserved, it should be separated from here into the prostate capsule and dissected at the "intrafascial" level. For dissociation close to the prostate capsule, absorbable biological clips and scissors can be used to avoid the use of energy devices such as ultrasonic scalpels and bipolar forceps to reduce electrical and thermal damage to the vascular nerve bundles. After completely cutting off the ligaments on both sides of the prostate, only the tip of the prostate remains connected.
Preserve distal urethra
The corpus cavernosum can be observed after dissection of the deep dorsal vein complex. At this time, the urethra can be withdrawn from the urethra. It can be observed that the urethra becomes empty after the urethra is withdrawn, further confirming the position of the urethra. If both sides of the prostate are fully freed, the prostate can be turned 180° to more completely remove the prostate tip behind the urethra and reduce the positive rate of the resection margin at the tip. Use scissors to sharply incise the anterior wall of the urethra close to the prostate. A urethra can be inserted to determine the position of the urethra, and the side and posterior walls of the urethra are exposed and cut off. Clamp the tip of the prostate and pull it upward to expose the urethrorectalis muscle behind the gland. Cut it from the side or retrogradely close to the prostate capsule. This part is close to the rectum and should be observed clearly to avoid damaging the posterior rectum. The distal urethra of the prostate should be kept as long as possible to facilitate urethral reconstruction and postoperative urinary continence recovery.
Anastomose urethra
Use 3-0 self-fixing absorbable thread, the needle arc is 1/2, the circumference is 26mm, the length is about 20~25cm, and the end is tied with 3~4 knots. First, suture the posterior wall of the bladder neck at 5 o'clock, 6 o'clock, 7 o'clock, and 9 o'clock from outside to inside, and then anastomose the corresponding points of the urethra from inside to outside. After the posterior wall of the bladder neck and the urethra are anastomosed with four stitches, the anastomosis line of the posterior wall is tightened. At this time, the urinary catheter is placed in the bladder, and the balloon is temporarily not filled with water. Continue to suture the bladder neck at 11 o'clock, 1 o'clock, 3 o'clock, and 5 o'clock to anastomose with the corresponding points of the urethra, tighten the sutures, and inject water into the urethra balloon. A total of 8 stitches were made. After that, the anterior bladder wall is suspended. The specific method is: after the urethral anastomosis is completed, continue to use the needle and thread that anastomoses the urethra to suture the anterior bladder wall muscle layer at 11 o'clock on the bladder neck, and then suture the original deep dorsal vein complex with a reverse needle. , suture the anterior bladder wall muscle layer at 1 point of the bladder neck again, and use biological clips to fix the end of the line to complete the anastomosis. Using this method to reconstruct the front of the anastomosis is simple and easy, reduces the tension of the anastomosis, and reduces the probability of postoperative anastomotic leakage; it also avoids knotting and simplifies the surgical operation.
Transabdominal route
Laparoscopic radical prostatectomy through the abdominal approach requires opening the retropubic prevesical space (Retzius space) close to the abdominal wall and dissociating it to the surface of the prostate. The remaining steps are similar to those of laparoscopic radical prostatectomy via extraperitoneal approach.
Operation skills
1. Precautions for establishing extraperitoneal cavity
To avoid damaging the peritoneum when establishing an extraperitoneal space, a longitudinal incision of 3 to 4 cm can be made below the umbilicus, and the anterior rectus abdominis sheath is transversely incised at two transverse fingers below the umbilicus. After the bilateral rectus abdominis muscles are seen, the index finger is placed close to the abdomen. Behind the rectus muscle, it expands in front of the posterior sheath of the rectus abdominis and the arcuate border. The midline can be pushed open with the index finger to merge the retroperitoneal spaces on both sides.
2. How to judge the bladder neck-prostate junction
There are three ways to judge the junction between the bladder neck and the prostate: ① Move the urinary catheter back and forth repeatedly, and roughly judge the bladder-prostate junction through the position of the urinary sac; ② The place where the fat on the front surface of the prostate ends roughly represents the prostate-vesical junction; ③ The change in the texture of the grasper can also help identify the bladder-prostate junction. The bladder is a hollow organ with a soft texture, while the prostate is a solid organ with a tough texture. Observe carefully at 12 o'clock, you can see that the space where the horizontal bladder fat terminates and the longitudinal lobes on both sides of the prostate meet to form a "cross", and the periprostatic fascia is cut transversely at the intersection of the "cross".
- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- 【4K Basics】4K Ultra HD Endoscope Camera System
- 【General Surgery Laparoscopy】"Two-step stratified method" operation flow of left lateral hepatic lobectomy
- 【General Surgery Laparoscopy】Left Hepatectomy